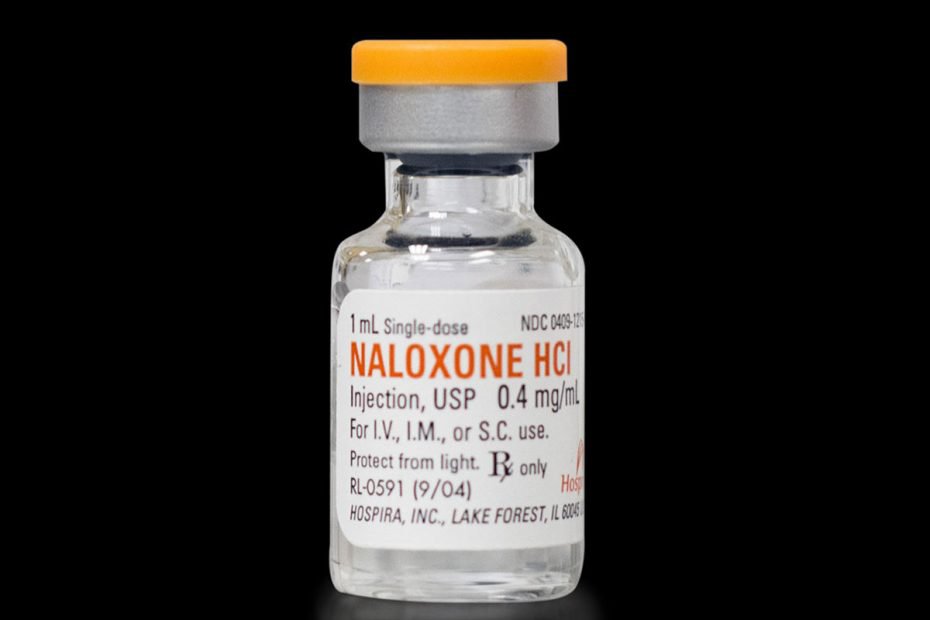
What does it look like?
Naloxone comes as a nasal spray, pre-filled syringe and ampoules.
Other names
Naloxone is commonly known as ‘Narcan®’.
Other types of opioids
- Buprenorphine
- Codeine
- Fentanyl
- Heroin
- Methadone
- Opium
- Oxycodone
How is naloxone used?
Naloxone is easy to use. And instructions are included with the product. The pharmacist can also provide information on how to administer naloxone.2
To use naloxone, firstly administer the naloxone and then call 000 for an ambulance. It is important to call 000 as naloxone only last for between 30 and 90 minutes and the person can overdose again when it wears off.2
Effects of naloxone
The effects of naloxone are to temporarily block opioid receptors and prevent opioid drugs from working. Naloxone cannot be used to get high, so it has no potential for non-prescribed use.
There is no evidence that extended use of naloxone can cause harmful physical effects or dependence. People who take naloxone do not develop a tolerance to its effects and there have been no reported deaths from naloxone overdose.3, 4
Side effects
Most side effects from naloxone are mild. However, if someone is opioid-dependent and they are given a high dose of naloxone, it can bring on symptoms of opioid withdrawal4 such as:
- nausea and vomiting
- sweating
- trembling
- nervousness
- fast pulse.4
In rare cases, even a person who is not opioid-dependent might experience:
- an allergic reaction with symptoms such as swelling of the face, lips, tongue and throat, wheezy breathing, chest tightness, intense rash with itching
- high blood pressure
- irregular heartbeat
- seizures.4
Naloxone and opioid overdose
People who have been revived with naloxone after overdosing on opioids may experience a strong urge to take more opioid drugs, especially if they are dependent.
Taking opioid drugs after naloxone is very dangerous. Naloxone only stays in the body for a short period of time (30 - 90 minutes) whereas heroin and other opioid drugs stay in the body for much longer. The effects of sustained-release opioids like OxyContin® and MS Contin® can last for over 12 hours, so naloxone will wear off long before the opioid has left the system. This means that taking more opioids after taking naloxone could cause a second overdose.5
For information about naloxone training and accessibility in your state or territory, get in touch with peak harm minimisation bodies or check the Pennington Institute to find out what local service providers are delivering training.
If your use of alcohol or other drugs is affecting your health, family, relationships, work, school, financial or other life situations, or you’re concerned about a loved one, you can find help and support.
Call the National Alcohol and Other Drug Hotline on 1800 250 015 for free and confidential advice, information and counselling about alcohol and other drugs
Help and Support Services search
Find a service in your local area from our list. Simply add your location or postcode and filter by service type to quickly discover help near you.
If you're looking for other information or support options, send us an email at druginfo@adf.org.au
Path2Help
Not sure what you are looking for? Try our intuitive Path2Help tool and be matched with support information and services tailored to you.
Find out more
- Brands. B., Sproule B, & Marshman J. Drugs & Drug Abuse. 3rd ed. Ontario: Addiction Research Foundation; 1998.
- Australian Government Department of Health. How to administer naloxone 2022 [cited: October 2022].
- Petty J, McNally S, Ryan J. Saving lives: Australian naloxone access model. Melbourne: Penington Insitute; 2018.
- Upfal J. Australian Drug Guide. 8th edition ed. Victoria: Griffin Press; 2016.
- Penington Institute. Overdose Basics Melbourne: Penington Institute; 2020 [cited 2020 March 12, ].