May 19, 2020
Fentanyl in the Australian illicit drug market
Fentanyl is a synthetic opioid that has gained significant attention in the last ten years along with growing global concern around opioid dependence.
Synthetic opioids, such as fentanyl, can be up to 100 times more potent than morphine.2,3
Recent media has reported increased concerns about fentanyl being found in various illicit drugs in Australia.1
Why is fentanyl a problem?
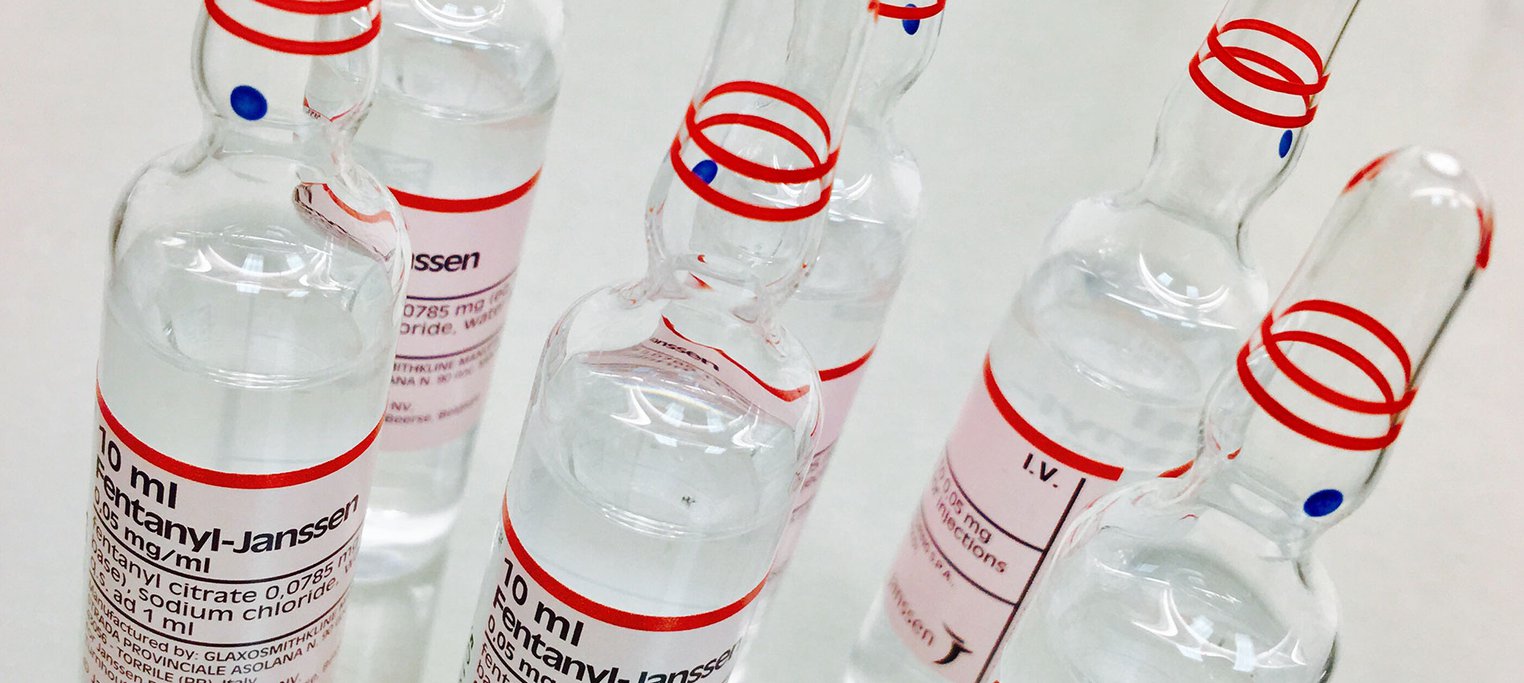
Fentanyl is commonly used for pain management in clinical settings.
It is now showing up, however, in some illicit drugs, including other opioids, around the world - in particular North America and Canada, where it has been found in samples of drugs, such as heroin.4
One of the reasons that fentanyl is becoming more common in the illicit drug market is its much stronger effect and its low price.5
The mixing of fentanyl into other opioid drugs is one of the reasons for an increase in opioid-related overdose deaths, 4 especially when the person taking the drug is unaware of fentanyl’s presence.
In the U.S alone there was a sixfold increase in overdose deaths in 2016, with up to 58% involving the illicit use of fentanyl in the north-eastern region of the US.6 Although not as significant, in 2013 it was reported that the majority of deaths associated with fentanyl in Australia involved illicit use.2
The Australian illicit drug market
There has been mounting concern from Australian health authorities about the recent contamination of drugs sold as cocaine and methamphetamine also containing fentanyl and acetyl-fentanyl.1
This means that people who are using what they think are stimulants are also inadvertently using one of the strongest forms of opioid available.
Acetyl-fentanyl is an analogue of fentanyl that is produced illegally and is not used in health care.
Health authorities in NSW issued warnings to the public in February this year, after several people presented to emergency rooms suffering from symptoms of opioid toxicity as a result of consuming powdered fentanyl and acetyl-fentanyl accidentally, thinking that they actually took stimulant drugs.1,7,8
Who is at most risk?
If fentanyl is introduced into drugs, such as heroin (even in small doses), and the person using it is not aware, this significantly increases their risk of accidental overdose.5
As methamphetamine and cocaine are both stimulants, it is unlikely that the people using these drugs would even suspect that synthetic opioids could be present.
Even though the illicit drug market is not regulated, it has been recognised by experts that the recent cases in NSW present a much higher risk to the health of the consumer due to the potency of fentanyl and acetyl-fentanyl.8
What can be done?
Drug experts have been expecting an increase in the presence of fentanyl in the Australian illicit drug market for some time,8 with many experts suggesting that Australia typically follows the patterns of drug harms that occur in countries such as Canada and the USA.8
For this reason, it is recommended that proven harm reduction strategies are implemented in Australia to prevent further overdoses relating to fentanyl.
Aside from raising general awareness of this risk7, other strategies such as the distribution of rapid fentanyl testing strips, and community education and training in the use of naloxone for people at risk of opioid overdose could be implemented.8
Rapid fentanyl testing strips are used to detect the presence of fentanyl in a drug, not quantity or strength. Programs that provide rapid tests have been demonstrated to be highly accurate and easy to use in trials in the US.6,8 The majority of participants that took part in this trial reported positive changes in drug use behaviour as a result, in that they decided not to consume drugs that tested positive for the presence of fentanyl.6,8 The introduction of testing strips may assist in reducing the unintended harms already witnessed in NSW.
Naloxone is a drug that temporarily reverses the effects of opioid drugs, such as heroin and fentanyl. It works by blocking opioid receptors in the brain, allowing the person who is experiencing the effects of opioids to recover normal respiratory function and regain consciousness.
There are many challenges to overcome, however, in ensuring that the people most at risk - who are not exposed to conventional channels of information or support services - are aware of the problem or know how to access fentanyl testing strips or naloxone.
Naloxone access in Australia
Peer to peer naloxone programs in communities with high illicit drug use have been shown to significantly reduce opioid-related overdose deaths.9
This is where people who use similar drugs are taught how to administer naloxone in the case of an overdose, and are provided with access to it.9
The Australian Government has initiated a take-home naloxone pilot program, which started in December 2019 and will run to February 2021.10
This program provides free, over-the-counter naloxone to people who are at risk of opioid overdose or adverse reaction, as well as their partners/families/friends and relevant community health care providers.10
The program is running across NSW, SA and WA and will provide important information about increased access to naloxone in an Australian setting.10
Although the recent harms reported in NSW were as a result of people taking stimulants that were contaminated with acetyl-fentanyl, the wider introduction and use of naloxone may assist in reversing future unintended opioid overdoses.
Further information
The presence of fentanyl within the illicit drug market in Australia is of increasing concern.
Communities need to be equipped with a range of prevention and harm reduction methods to help reduce the risk of overdose and death.
Call the National Alcohol and Other Drug Hotline on 1800 250 015 for free and confidential advice, information and counselling about alcohol and other drugs
You can also access information about different types of illicitly used drugs on ADF’s Drug Facts pages.
Aubusson K. Sydney drug users poisoned by fentanyl believing it's cocaine. The Sydney Morning Herald. 2020.
Roxburgh A, Burns L, Drummer OH, Pilgrim J, Farrell M, Degenhardt L. Trends in fentanyl prescriptions and fentanyl‐related mortality in Australia. Drug and Alcohol Review. 2013;32(3):269-75.
National Drug and Alcohol Research Centre. Powerful opioid fentanyl poses serious risk of fatal overdose NSW: NDARC; 2020 [cited 2020 March, 19]. Drug Enforcement Administration, U.S. Department of Justice. Drugs of Abuse 2017 Edition: A DEA Resource Guide. USA; 2017.
National Institute on Drug Abuse. Drug Facts: Fentanyl USA: NIDA; 2019 [cited 2020 March, 19].
Goldman JE, Waye KM, Periera KA, Krieger MS, Yedinak JL, Marshall BD. Perspectives on rapid fentanyl test strips as a harm reduction practice among young adults who use drugs: a qualitative study. Harm Reduction Journal. 2019;16(1):3.
Health NDo. Warnings over fentanyl risk in Sydney NSW: NSW Department of Health; 2020 [cited 2020 March, 19].
Allan J. The deadly opioid fentanyl is turning up in disguise on Sydney streets, making illicit drug use even riskier NSW: The Conversation; 2020 [cited 2020 March, 19].
Hanson BL, Porter RR, Zöld AL, Terhorst-Miller H. Preventing opioid overdose with peer-administered naloxone: findings from a rural state. Harm Reduction Journal. 2020;17(1):1-9.
Australian Government Department of Health. About the take home naloxone pilot Canberra: Australian Government Department of Health; 2019 [cited 2020 March, 19].