How is fentanyl used?
Pharmaceutical fentanyl can be taken in many different ways, including via nose (nasal spray), mouth (pills or tablets that dissolve in your mouth), injection and skin (patches).6
While there are patches specifically formulated for absorbing fentanyl through the skin, other forms can’t be used this way and you won’t experience the effects or overdose just by touching them.8
lllegally made fentanyl can be swallowed, injected, smoked or snorted.2
Effects of fentanyl
Use of any drug can have risks – prescription or illegal. It’s important to be careful when taking any type of drug.
Fentanyl affects everyone differently, based on:
- size, weight and health
- whether the person is used to taking it
- whether other drugs are taken around the same time
- the amount taken
- the strength of the drug (varies between drug form e.g. patches, lozenges or injection and from batch to batch for illegally made fentanyl).
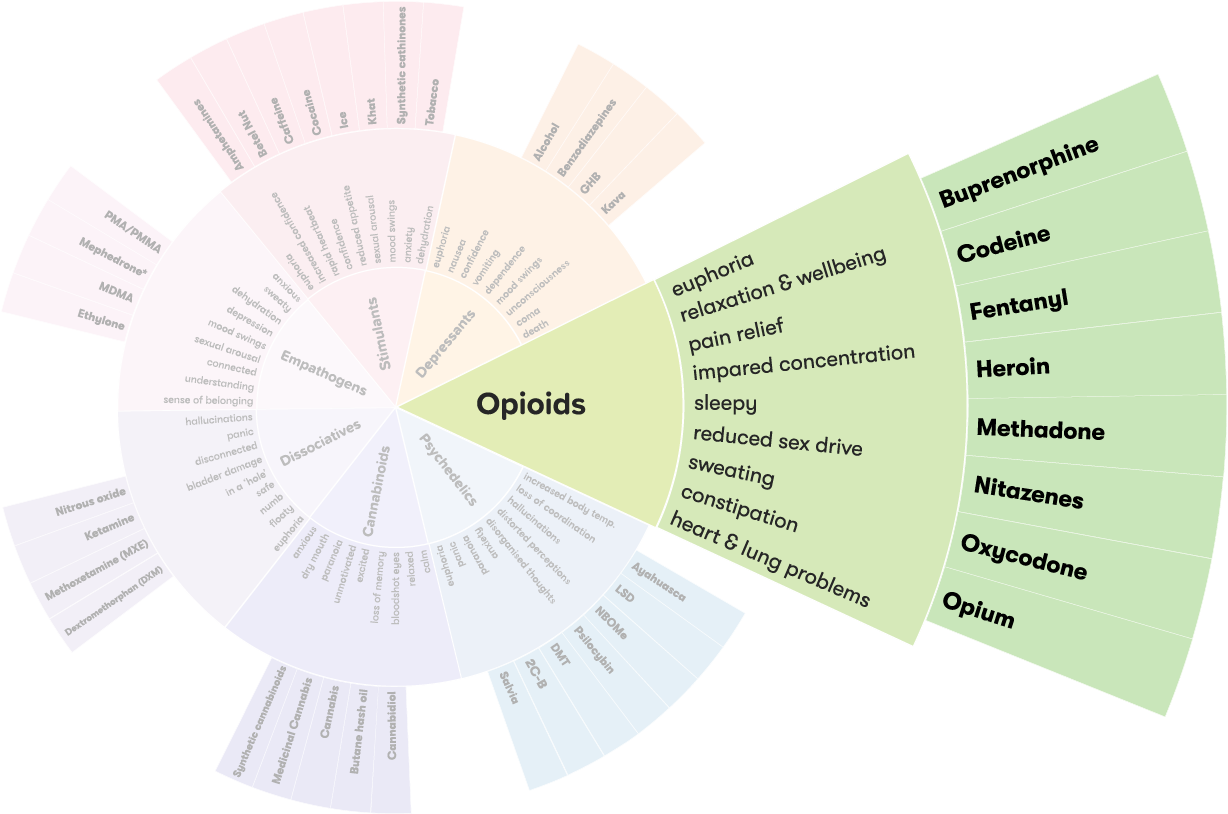
Its effects may include:
- pleasure, feelings of happiness (euphoria)
- pain relief
- upset stomach, nausea, vomiting
- constipation or diarrhoea
- wind, indigestion, cramps
- drowsiness, confusion
- weakness or fatigue
- headache
- incoherent or slurred speech
- dizziness, impaired balance
- slow pulse, lowered blood pressure
- rash (inflammation, itch, swelling) from the skin patch. 5,9,10
If injecting drugs, there is an increased risk of:
- tetanus
- infection
- vein damage.11
If sharing needles, there is an increased risk of:
- hepatitis B
- hepatitis C
- HIV and AIDS.11
Overdose
If the dose is too high, or you take fentanyl without knowing it, you could overdose.
Fentanyl overdose can cause death. Call an ambulance straight away by dialling triple zero (000) if you or someone else has any of these symptoms (emergency services are there to help and can provide instructions over the phone):
- slow/shallow breathing
- bluish/greyish lips and complexion
- passing out
- coma
- death.5,12
Naloxone (also known as Narcan®) temporarily reverses the effects of opioid overdose (including fentanyl). 13
It’s available for free over the counter from your local pharmacy and can be administered by anyone, including family or friends and bystanders.14
Long-term effects
Regular, long-term use of fentanyl may cause:
- dependence
- less effective pain relief (tolerance)
- increased risk of getting sick from viruses and infections
- sleep problems
- reduced bone density and higher risk of breaking bones
- heightened sensitivity to pain (opioid-induced hyperalgesia)
- impacts on hormone levels leading to reduced sex drive, infertility, erectile dysfunction, or menstrual cycle changes.15-17
Fentanyl and mental health
It’s common for people using illicit opioids to experience mental health problems at some point in their lives. This doesn’t mean that using opioids causes mental health problems. For some people, fentanyl is used to help them cope with symptoms of mental ill-health.
In some cases, the side effects of long-term fentanyl use (like sleep difficulties) can lead to people developing mental health issues.10
More than half of those who use illicit opioids report experiencing symptoms of a mental illness at some point in their lives, most commonly depressive and anxiety disorders.10 More than 40% of people who use illicit opioids experience symptoms of PTSD.10
Up to half of people who use illicit opioids have experienced childhood trauma.10
Tolerance and dependence
People who regularly use fentanyl can become dependent on it. They may feel they need fentanyl to go about their normal activities like working, studying and socialising, or just to get through the day.
They may also develop a tolerance to it, which means they need to take larger amounts to get the same effect.
Using fentanyl with other drugs
The effects of taking fentanyl with other drugs – including over-the-counter or prescribed medications – can be unpredictable and dangerous.
- Opioids + cannabis: can work together to increase effects, so while the risk is low there is still a possible risk.
- Opioids + anti-depressants: There have been rare reports of a risk of serotonin syndrome when using SSRIs. There have also been rare reports of severe and varied reactions from MAOIs.
- Opioids + nitrous oxide: can cause impaired coordination, memory loss and passing out.
- Opioids + GHB/GBL/benzodiazepines/alcohol: can cause difficulty breathing, passing out, vomiting and possible death.
- Opioids and ketamine: can cause nausea, vomiting, passing out and possible death.
- Opioids and cocaine/ice/speed: increases the risk of heart strain. The stimulant effect of cocaine increases heart rate, and the opioids decreases heart rate. There is a risk of breathing or heart problems if one drug wears off before the other.18,19
More on Polydrug use
Polydrug use is a term for the use of more than one drug or type of drug at the same time or one after another. Polydrug use can involve both illicit drugs and legal substances, such as alcohol and medications.
Reducing harm
- If prescribed, follow the directions given to you by your doctor or pharmacist. Don’t stop using your medicine or lower the dose without checking with your doctor.
- Don’t take fentanyl with other opioids or depressants, this increases the risk of overdose
- Always carry naloxone and encourage family and friends to also carry it
- Avoid driving or operating machinery after use
- Fentanyl patches should be stored out of reach of children, at room temperature, and away from excess heat and moisture (not in the bathroom). To dispose of used patches, fold it inwards on itself so the sticky sides meet, wrap in plastic or paper and put in the rubbish
- If injecting, use new needles and sterile injecting equipment to avoid blood borne viruses
- Fentanyl may unknowingly be in or be sold as other drugs, such as cocaine or MDMA:
- use in a safe place with people you trust and can help if needed
- ‘start low, go slow’: try a small amount first and wait a while to see how you are affected
- use drug checking (pill testing) services, where available. If there is no drug checking service near you, your local needle and syringe program (NSP) may have fentanyl test strips.
- check for drug alerts related to the drug you are taking.2,15,18,20
Withdrawal
Giving up fentanyl after a long time is challenging because the body has to get used to functioning without it.
Seek advice from a health professional before stopping fentanyl as they can help you slowly reduce your dose (taper), or access opioid pharmacotherapy. This can help reduce withdrawal symptoms or prevent them from occurring.
Withdrawal symptoms usually start within 12 hours after the last dose and can last for about a week. Days one to three will be the worst. Symptoms include:
- goose flesh/bumps
- bouts of chills alternating with bouts of flushing and excessive sweating
- irritability
- insomnia
- loss of appetite
- yawning and sneezing
- watery eyes and runny nose
- vomiting and nausea
- diarrhea
- increased heart rate and blood pressure
- pains in the bones and muscle
- general weakness
- depression.9,21
Getting help
If your use of fentanyl is affecting your health, family, relationships, work, school, financial or other life situations, or you’re concerned about a loved one, you can find help and support.
Call the National Alcohol and Other Drug Hotline on 1800 250 015 for free and confidential advice, information and counselling about alcohol and other drugs
Help and Support Services search
Find a service in your local area from our list. Simply add your location or postcode and filter by service type to quickly discover help near you.
If you're looking for other information or support options, send us an email at druginfo@adf.org.au.
Path2Help
Not sure what you are looking for? Try our intuitive Path2Help tool and be matched with support information and services tailored to you.
Find out more
Using or possessing fentanyl without a prescription from a doctor, or selling or giving fentanyl to someone else, is illegal. There are also laws against forging or altering a prescription or making false representation to get a fentanyl prescription.
Fentanyl is a schedule 8 Drug.22 Doctors must follow additional state and territory laws when prescribing fentanyl and must notify, or receive approval from, the appropriate health authority.
See also, drugs and the law.
Between 2001 and 2021 there were 833 fentanyl deaths reported in Australia. 774 of these deaths were caused by pharmaceutical fentanyl, and 37 were caused by illegally made fentanyl and fentanyl analogues.4
The rate of fentanyl deaths decreased from 2015-2021, which may be due to a number of factors including less prescribing and the release of tamper resistant oxycodone.4
As of 2018, recent fentanyl injection was reported by 8% of people who inject drugs in Australia.23 Those who had injected fentanyl were more likely to inject daily or more frequently, have overdosed in the past year, or identify as Indigenous Australian.23,20,15,20
- John Hopkins Medical. What are opioids? 2024 [12.01.2021].
- National Harm Reduction Coalition. Fentanyl Use and Overdose Prevention Tips. 2024 [22.10.2024].
- Piatkowski T, Kill E, Reeve S. ‘The gear could be cut with fentanyl which is starting to happen more in Australia’: exploring overdose survivors’ perspectives on toxic supply and safe consumption.Drugs: Education, Prevention and Policy [Internet]. 2024 [15.11.2024]:[1-9 p.].
- Roxburgh A Nielsen S. Twenty-year trends in pharmaceutical fentanyl and illicit fentanyl deaths, Australia 2001–2021. International Journal of Drug Policy [Internet]. 2022 [31.03.2023]; [109p.].
- Upfal J. Australian drug guide: the plain language guide to the top 300 drugs and medicines, plus more. Collingwood, Vic.: Black Inc.; 2022
- Health Direct. Fentanyl. 2024 [22.10.2024].
- Comer SD, Cahill CM. Fentanyl: Receptor pharmacology, abuse potential, and implications for treatment. Neuroscience & Biobehavioural Reviews [Internet]. 2020 [20.11.2024]; (106):[49-57 p.].
- Feldman R, Weston BW. Accidental Occupational Exposure to a Large Volume of Liquid Fentanyl on a Compromised Skin Barrier with No Resultant Effect. Prehospital and Disaster Medicine [Internet]. 2022 [31.10.2024]; 37(4):[550-2 p.].
- Fust K. "Fentanyl." The Gale encyclopedia of prescription drugs: a comprehensive guide to the most common medications.Farmington Hills, Mich: Gale, Cengage Learning; 2015 [22.10.2024]. Available from:
- Darke S, Lappin J, Farrell M. The clinician's guide to illicit drugs and health: Silverback Publishing; 2019.
- Tran LT, Peacock A, Colledge S, Memedovic S, Grebely J, Leung J, et al. Injecting risk behaviours amongst people who inject drugs: A global multi-stage systematic review and meta-analysis. International Journal of Drug Policy [Internet]. 2020 [16.10.2024]; 84p.].
- Medline Plus. Fentanyl Transdermal Patch. U.S. Department of Health and Human Services; 2020 [31.10.2024].
- Victoria State Government Department of Health. Victoria's Take-Home Naloxone Program. 2024 [18.09.2024].
- Australian Government Department of Health and Aged Care. About the Take Home Naloxone program. 2024 [16.10.2024].
- NPS MedicineWise. Fentanyl Sandoz. 2020 [1.11.2024]. Available from:
- NPS MedicineWise. Opioid medicines and chronic non-cancer pain. 2021 [31.10.2024].
- Kotlińska-Lemieszek A, Żylicz Z. Less Well-Known Consequences of the Long-Term Use of Opioid Analgesics: A Comprehensive Literature Review. Drug design, development and therapy [Internet]. 2022 [15.11.2024]; 16:[251-64 p.].
- Hi-Ground. Opioids n.d. [05.01.2022].
- Psychonaut Wiki. Fentanyl 2022 [17.01.2023].
- NPS MedicineWise. Accidental fentanyl exposure in children can be fatal. 2015 [1.11.2024].
- Brands B, Sproule B, Marshman J. Drugs & drug abuse: Toronto: Addiction Research Foundation; 1998
- Australian Government Department of Health and Aged Care TGA. Scheduling basics of medicines and chemicals in Australia. n.d. [31.10.2024].
- Geddes L, Iversen J, Memedovic S, Maher L. Intravenous fentanyl use among people who inject drugs in Australia. Drug and Alcohol Review [Internet]. 2018 [15.11.2024]; 37:[S314-S22 p.].