Opioids

Last published: June 06, 2024
What are opioids?
Opioids include any drug that acts on opioid receptors in the brain, and any natural or synthetic drugs that are made from or related to the opium poppy.
Opiates are a type of opioid. They’re drugs which are naturally derived from the opium poppy plant, and are not synthetic.1
The opioid receptor system
Opioids bind to opioid receptors which depress the central nervous system – meaning they slow down messages between the brain and the rest of the body.
On opioids, your breathing and heart rate slow down. Dopamine is released, causing sensations of pleasure and pain relief.2
If breathing and heart rate slow down too much, breathing may stop, leading to an overdose.3 Opioid overdose can result in death and other injuries. But, it can be reversed by CPR and naloxone administration.3, 4
Naloxone is a drug that also binds to opioid receptors, but has the opposite effect. It blocks the receptors from attaching to other opioid drugs, so it can reverse an overdose.
Naloxone is used in Australia in clinical and ambulance settings, and has recently been made available over the counter.
How are opioids used?
Opioids can be used in various ways. Opioid-based medications are usually found in tablet form and are often swallowed.
Opiate-substitution treatment (pharmacotherapy) is found in liquid, tablet and film formations and is used via mouth and by dissolving the film under the tongue.
Heroin is usually injected but is also snorted or smoked.
Commonly used opioids
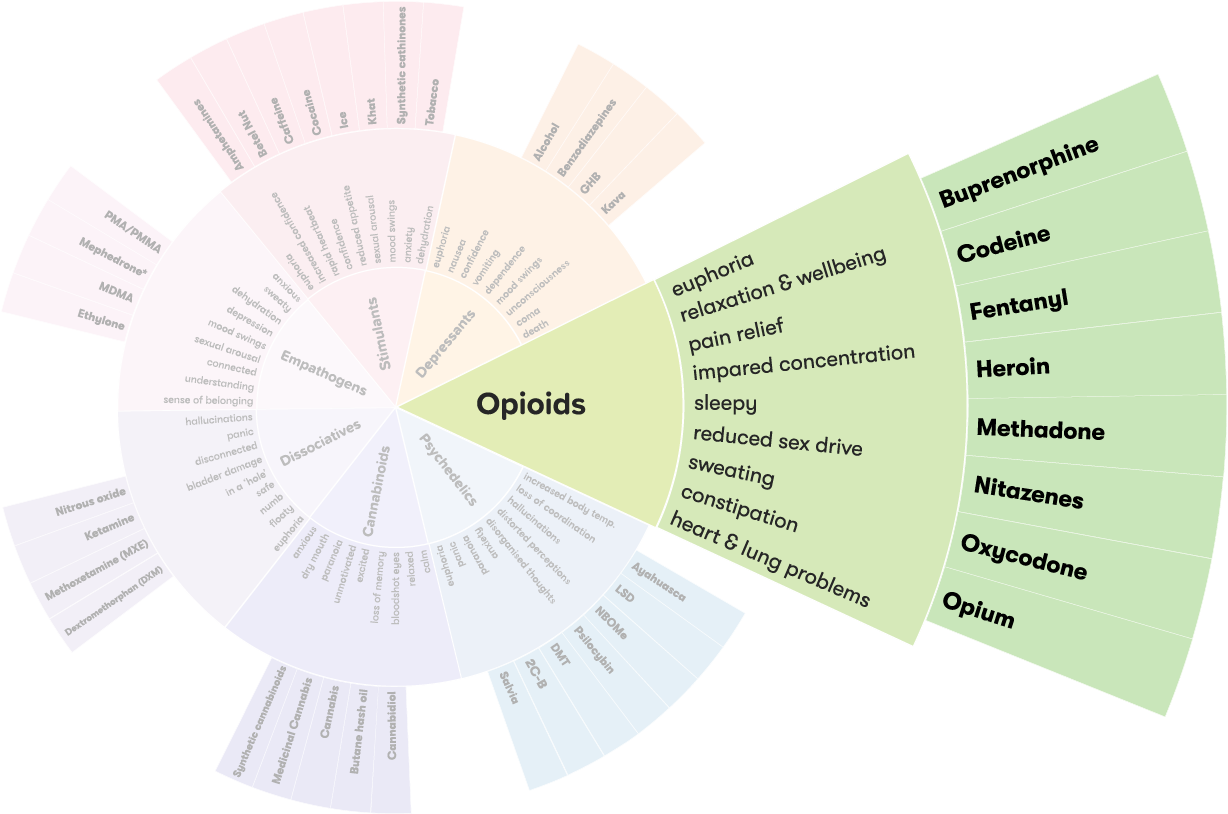
Explore opioids on the Drug Wheel
Types of commonly used opioids
General
Opioids include certain types of pain killers, known as ‘opioid pain medications’ and illegal drugs, such as heroin. Some opioids are plant-based and come from the opium poppy (opiates), while others are synthetic or ‘man-made’.
Opioid-based medications
Common types of opioid-based medications include codeine (Panadeine®, Panadeine Forte® and Nurofen Plus®), fentanyl, morphine, oxycodone (Endone® or OxyContin®), buprenorphine (Subutex® or Suboxone®), methadone and tramadol. They act in the same way as other opioids such as heroin to produce feelings of pain relief.
Opioid-based medications are commonly prescribed by doctors, and up until 2018 some lower strength opioids were available to buy over the counter in Australia. However opioid-based medications are now only available with a prescription.
Many people don’t realise that some medications prescribed for pain relief can cause dependence. If they are overused or combined with other depressant drugs, such as alcohol or benzodiazepines, they may also cause overdose.
Pharmaceutical opioids now account for more drug-related deaths in Australia than any other drug category.3
Heroin
Heroin is the common name for diecetylemorphine or diamorphine. Diamorphine is used in clinical settings and is used in prescription heroin programs internationally. Heroin is an opiate, meaning it comes from the opium poppy.4
Opiate substitution treatments
Methadone (Methadone Syrup® and Biodone Forte®) and buprenorphine (Suboxone® or Subutex®) are opioid-based medications used to treat dependence on heroin or other opioids. It’s also known as pharmacotherapy or opiate substitution treatment (OST).
OST is prescribed by a doctor to help people using opioids to reduce or stop their use. They manage cravings and withdrawal symptoms. Methadone is also used in clinical settings following heart attacks, trauma and surgery.
Newer psychoactive opioid substances
Newer psychoactive opioid substances include U-47700, AH-7921, O-desmethyltramadol, MT-45, acetylfentanyl and furanyl-fentanyl. These opioids have a very short history of human use and not much is known about the toxicity and potential for dependence.
It’s highly recommended to be very cautious and use harm reduction practices if using any of these substances.
Naloxone
Naloxone is classified as an opioid as it binds to opioid receptors, but it acts in the opposite way of most opioids. Naloxone blocks other opioids from binding to receptors, and can reverse opioid overdoses within minutes.
It does not have the same effect as other opioids and does not produce feelings of pain relief and pleasure.
Naloxone is only useful to reverse overdoses of other opioids, and will not effect overdoses due to alcohol, benzodiazepines, stimulant or hallucinogenic drugs, or non-opioid based medications.
Effects of opioids
Use of any drug can have risks. It’s important to be careful when taking any type of drug.
Opioids effect everyone differently, based on:
- the person’s size, weight and health
- whether the person is used to taking it
- whether other drugs are taken around the same time
- the amount taken
- the strength of the drug.
Effects of opioids include:
- extreme relaxation
- drowsiness and clumsiness
- confusion, slurred speech,
- slow breathing and heartbeat.5
If a large dose is consumed, effects may include:
- cold, clammy skin
- slow breathing
- blue lips and fingertips
- falling asleep (‘going on the nod’)
- death by respiratory depression.5
Long-term effects include:
- increased tolerance
- constipation
- dependence
- damage to vital organs such as the lungs, brain and heart.5
Using opioids with other drugs
The effects of taking opioids with other drugs – including over-the-counter or prescribed medications – can be unpredictable and dangerous, and could cause:
Opioids + alcohol, cannabis or benzodiazepines: slow down breathing and brain activity, and increased risk of overdose.6
Opioids + ice, speed or ecstasy: enormous strain on the heart and kidneys, and increased risk of overdose.7
More on Polydrug use
Polydrug use is a term for the use of more than one drug or type of drug at the same time or one after another. Polydrug use can involve both illicit drugs and legal substances, such as alcohol and medications.
Reducing harm
Use of opioids is likely to be more dangerous when:
- combined with alcohol or other drugs, in particular benzodiazepines or other opioids, as these can slow breathing and increase the risk of overdose6
- driving or operating machinery, as a person’s ability to judge distance and space is extremely limited
- a person is alone (in case medical assistance is required). It’s recommended that an unaffected person is present incase assistance is required
- injecting equipment is not sterile.
If you or someone you know is using opioids, it would be a good idea to talk with your doctor about accessing naloxone, the drug that reverses opioid overdoses. Your friends or family members can be trained in overdose reversal in case of an emergency.
More information at Harm Reduction Victoria.
Pain management plans
If you’re prescribed opioid-based medications, ask your doctor about a ‘pain management plan’, and other non-medicine (such as physical therapy) and non-opioid strategies (such as paracetamol) you can use to complement your treatment and reduce your reliance on opioid-based medications.
Tolerance and dependence
There’s evidence that after using them for a long time, many drugs can cause dependence. People who use opioids regularly can develop dependence and tolerance to it. This means they need to take larger amounts of the drug to get the same effect.
Dependence on a drug can be psychological, physical, or both. People who are dependent on a drug find that using it becomes far more important than other activities in their life. They crave the drug and find it very difficult to stop using it.
People who are psychologically dependent on a drug may feel the urge to use it when they are in specific surroundings, such as socialising with friends.
Physical dependence occurs when a person’s body adapts to a drug and gets used to functioning with the drug present.
Getting help
If your use of opioids is affecting your health, family, relationships, work, school, financial or other life situations, or you’re concerned about a loved one, you can find help and support.
Call the National Alcohol and Other Drug Hotline on 1800 250 015 for free and confidential advice, information and counselling about alcohol and other drugs
Help and Support Services search
Find a service in your local area from our list. Simply add your location or postcode and filter by service type to quickly discover help near you.
If you're looking for other information or support options, send us an email at druginfo@adf.org.au
Path2Help
Not sure what you are looking for? Try our intuitive Path2Help tool and be matched with support information and services tailored to you.
Find out more
- LiverTox.Opioids 2020 [cited: 07.04.2022].
- Hasan P Williams J. Basic opioid pharmacology: an update. British Journal of Pain 2012;6(1):11-6
- Pennington Institute.Overdose Basics 2020 [cited: 07.04.2022].
- Pennington Institute. Overdose Basics 2020 [
- NPS MedicineWise. Opioid medicines and chronic non-cancer pain 2021 [cited: 21.04.2022].
- U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning n.d. [cited: 21.04.2022].
- Goldsmith R Weisz M Shapiro H. The Essential Guide to Drugs and Alcohol 2010.